by Jeff Packer | Mar 10, 2024 | Change, Family, Health & Fitness, Mental Health, Stress
What I wouldn’t give to feel normal again! Sometimes we lay in bed and as we awake to our alarm clock, before moving an inch, we think we are going to feel normal again, pain-free. We roll over and as we attempt to get up, BAM! We are reminded by the strike of...
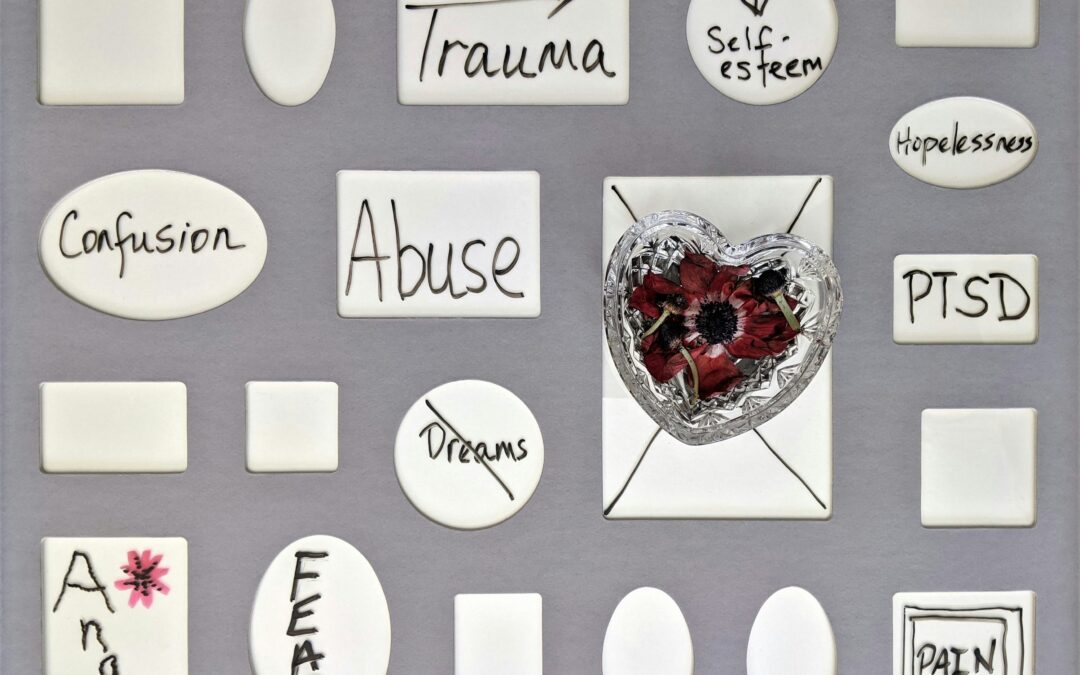
by Jeff Packer | Mar 6, 2024 | Anxiety, Change, Conflict, Crisis, Depression, Family, Grief, Mental Health, Problem-Solving, Stress, Trauma - PTS Reaction, Work & Employment
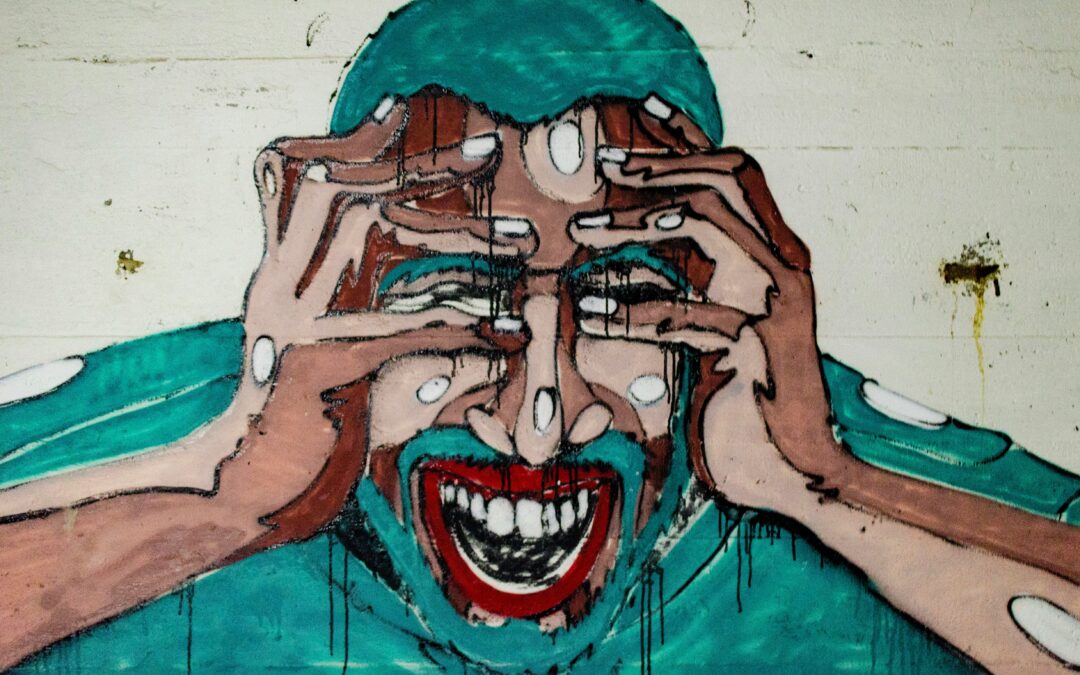
or… Post-Traumatic Stress “Reaction” (PTSR) “The anger, the rage, the hurt, and the cold loneliness that separates you from your family, friends, and society’s normal daily routine are so powerful that the option of destroying yourself is both real...

by Jeff Packer | Feb 22, 2024 | Anxiety, Conflict, Depression, Mental Health, Sexuality, Trauma - PTS Reaction
Horrendous secrets many people carry for months, years, decades and maybe even to their grave can lead to debilitating stress. This can result in what many people call a “break-down”. It was historically referred to as a “nervous breakdown”,...
![Shhhh…[Keeping Mental Health a Secret]](https://jeffpacker.com/wp-content/uploads/2013/09/marcel-strauss-fzqxoFJytiE-unsplash-1080x675.jpg)
by Jeff Packer | Feb 21, 2024 | Anxiety, Crisis, Depression, Health & Fitness, Love & Relationships, Mental Health, Stress, Teens
“Mental health concerns are dirty little secrets that should not be spoken about. They are problems that no one should know about except the immediate people that are affected. Mental health concerns show weakness and shame towards the family name. “ With thoughts...

by Jeff Packer | Jan 28, 2024 | Anxiety, Change, Depression, Mental Health, Stress
The Diagnostic Statistical Manual of Mental Disorders (DSM) identifies specific signs and symptoms required to be diagnosed with a major depressive disorder. However, there are many faces to depression, and one should not wait to meet all the criteria from the DSM to...

![Shhhh…[Keeping Mental Health a Secret]](https://jeffpacker.com/wp-content/uploads/2013/09/marcel-strauss-fzqxoFJytiE-unsplash-1080x675.jpg)

Recent Comments